In Nj Will Medicaid Pay for a Family Member to Take Care of You?
This guide volition answer common questions about how to use your Medicaid to become health care services. It will cover:
- Understanding Your Medicaid Plan
- Finding a Md
- Getting Care
- Appealing a Denial
Understanding Your Medicaid Program
Exercise I take Medicaid through "fee-for-service" or through a "managed care program"?
To start the process of getting health intendance services using your Medicaid, the beginning thing yous should know is whether you get your Medicaid direct through the city or state, called "fee-for-service Medicaid" or "straight Medicaid," or if you get your Medicaid through a private wellness insurance programme, chosen a "Medicaid managed care plan."
Yous tin figure this out by:
- Checking your Medicaid card(due south). Do yous have a card that says a program name similar Emblem Health, Healthfirst, or United Healthcare? If you do, and so you have Medicaid through a managed care plan.
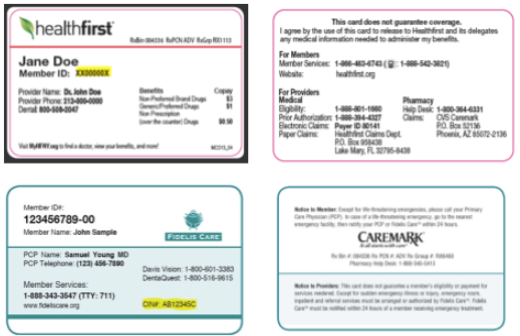
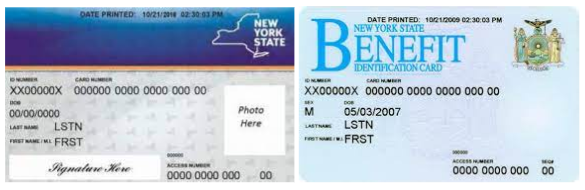
If the just Medicaid bill of fare y'all use is a New York State benefits card, y'all probably have fee-for-service or directly Medicaid. You lot should accept a carte that looks similar i of the cards beneath fifty-fifty if you also accept a programme card. NOTE: If you besides receive greenbacks assistance and/or SNAP (also known every bit food stamps), you use this carte du jour for those benefits likewise.
- Calling the New York Land of Health at 1-855-355-5777 or the New York City Human Resources Assistants Medicaid Helpline at 888-692-6116. Enquire if you are enrolled in a Medicaid managed care program. If they tell you lot that you are enrolled in a plan, be sure to inquire which i and get the telephone number for the plan.
I get my Medicaid through a "Medicaid managed intendance program." What is that and how does it work?
A Medicaid managed care plan is a individual health insurance programme that works with a group of doctors, clinics, hospitals and pharmacies to provide your care. This is called a "network." Yous can only meet these "in-network" doctors.
Y'all volition need to choose i of the doctors from the health program to be your primary intendance provider (PCP). Your PCP will provide nigh of your care. You may need a referral from your PCP to run across a specialist and for other services.
What wellness care services are covered by Medicaid?
Whether you go your Medicaid through a managed care plan or fee-for-service, Medicaid pays for all medically necessary covered services, including:
- Hospitalization
- Outpatient care
- Mental health care
- Concrete therapy
- Diagnostic tests
- Durable medical equipment (wheelchairs, orthotics, sure medical supplies, etc.)
- Prescription drugs
- Prenatal care
- Home intendance and nursing domicile care
- Limited dental care
- Transportation to medical appointments
Can I be charged for health intendance services that are covered by Medicaid?
If you go to a provider that takes your Medicaid, yous tin can only be charged limited co-payments for wellness care services that are covered past Medicaid. Some of these co-payments include:
- Clinic Visits: $three.00
- Laboratory Tests: $0.50
- Prescription Drugs: $1.00-$3.00
- Medical Supplies: $1.00
- Inpatient Hospital Stays: $25.00
- Emergency Room: $3.00
A provider can ship you a bill for whatever unpaid corporeality, but a provider cannot decline to give you a wellness care service if y'all cannot pay the co-payment, or if you have an outstanding balance from a prior visit.
Finding a Md
If I demand to find a principal intendance provider, dentist, or other health care provider that takes my Medicaid, what practise I do?
There are several ways you can find a wellness care provider in your area that takes your Medicaid plan:
- If you have a Medicaid managed care programme :
- Call the member services number on your insurance card, tell them what kind of provider you are looking for (like a primary care doctor, dentist, chemist's shop, or other specialist), and inquire them to send you a listing of in-network providers in your area or if they a have online provider search you tin can apply. You tin besides ask member services if particular providers are in your plan's network.
- New York State has a Provider "Lookup" tool that you tin apply to search for in-network providers. Go to the website, and enter your wellness insurance company, health plan, naught code, and number of miles you are willing to travel to this doctor. Click on "Advanced Search" to include a specific type of md (like a master care doctor, dentist, or other specialist).
- Notation: You may need to get a referral from your primary care provider before going to a specialist.
- If you have fee-for-service Medicaid :
- You can see any provider that accepts fee-for service Medicaid. To find providers who have fee-for-service Medicaid, use the New York Land Provider Lookup tool at this website.
Ever phone call the doctor earlier making an appointment to confirm that they accept your Medicaid.
My Medicaid managed care plan said I need to choose a main care provider, how practice I practice that?
If your Medicaid managed care plan says that you lot need to choose a primary care provider (PCP) and you already have an in-network provider that y'all want to be your main provider, all you have to do is call your plan and give them the name and contact information for that provider.
If you need to find a provider that you desire to exist your PCP, follow the steps in a higher place to find an in-network provider, call the provider's role to make sure that they are taking new patients, and and so call your plan and requite them the name and contact information for that provider as your new PCP.
You can change your PCP at any time by calling your programme and giving them the proper noun and data for your new provider of choice.
Remember, you must always chose an in-network provider. If you lot practice not choose your ain PCP, your program may assign you ane.
Getting Care
I take a doctor or specialist that takes my Medicaid, what do I exercise to get the care I need from them?
Make an appointment with your doctor. Be certain to bring your Medicaid card(s) and any other insurance cards you have with you to the appointment and requite them to the office receptionist earlier your visit. Bringing all your insurance cards with y'all and giving them to the role before every visit helps protect you from beingness accidentally billed.
If yous doctor decides that yous need a health care service, like a surgery, prescription drug, or dental filling, Medicaid may agree to pay for the service without whatsoever delay or actress paperwork. But some services require prior authorization, also called prior approval, before Medicaid will concord to pay for them.
What is prior authorization?
Some wellness care services are covered by Medicaid, but only if your provider proves that you lot come across sure criteria. This is chosen prior authorization, besides chosen prior approval. If a health care service requires prior say-so, your provider has to become permission from your Medicaid managed care plan or Medicaid fee-for-service before giving you the care or medication you demand. If your provider does non get this permission, Medicaid may not pay for it.
The Medicaid-covered services that require prior authorization are listed in your Medicaid managed care Fellow member Handbook. If your provider is telling you that a service is not covered or requires prior authorization, you tin can besides phone call your programme and ask.
If a health care service requires prior authorisation, your managed care programme, or the State Department of Wellness if yous take fee-for-service, will have criteria or standards that you must evidence you lot meet in order for you lot get the wellness care service from Medicaid. For example, your programme may only comprehend a more expensive brand proper name drug if your medico can prove why a less expensive generic drug does not work as well for you lot. Often, doctors are required to prove that the service you need is "medically necessary" for yous. This means that your doctor needs to show how the service is necessary to treat your medical status that is causing yous bug. For example, Medicaid will but "authorize" and pay for home care services for you if a md tin bear witness that yous cannot do activities of daily living on your own.
If a service that yous need requires prior authorization, your provider should enquire your programme or fee-for-service Medicaid what criteria you need to see to get blessing for the service. Then your provider should submit a prior authorization request to the plan or Medicaid fee-for-service explaining why and how you encounter those standards. Your doc should include whatsoever medical documentation and records that help prove this point.
If a delay in receiving the requested service would seriously damage your life or wellness, your provider should notation this and inquire for "expedited review".
How long does Medicaid have to make a decision on a prior authorization request?
After your provider submits a prior authorization asking, Medicaid must make a decision inside three business days of receiving all necessary information.
If your provider asked for and your Medicaid granted expedited review, Medicaid must brand a conclusion within 72 hours of receiving the request.
Medicaid tin can extend these deadlines to up to fourteen calendar days if more data was needed from you or your provider to make a decision.
What notice will I get if Medicaid approves my service?
If Medicaid approves your asking, you lot will receive written detect of the blessing in the mail. Your provider will also receive notice of the approving. Depending on how your provider receives notices, they may receive it in the mail or electronically.
Appealing a Denial
What find will I get if my Medicaid denies my service?
- If you take a Medicaid managed care plan and your plan denies your request, y'all will receive a written denial notice in the mail called an "Initial Adverse Determination." This find volition explicate why the plan denied your care and give you a deadline and instructions for appealing the deprival. Your provider will also receive notice of the denial. Depending on how your provider receives notices, they may receive it in the mail or electronically.
- If you have fee-for-service Medicaid and Medicaid denies your request, you will receive a written denial detect in the mail. This find will explain why Medicaid denied your care and give you a deadline and instructions for appealing the denial. Your provider will as well receive notice of the deprival. Depending on how your provider receives notices, they may receive it in the mail or electronically.
How do I appeal my Medicaid managed care plan's decision to deny my service?
Programme Entreatment
If you want to appeal your Medicaid managed intendance plan's decision to deny your service, you first have to file an appeal with your program called a Plan Appeal, also sometimes called an internal appeal. You have lx days from the date on the Initial Adverse Determination notice to request a Plan Appeal.
Instructions on how to request the Plan Appeal are included on the Initial Adverse Conclusion notice.
- Y'all can enquire your provider, a family member, an attorney, or anyone else you trust to help yous with the entreatment, yous just take to give them written permission on the appeal form.
- You can include additional data or paperwork with your appeal, like letters from your doctors explaining why you demand the service, medical records, x-rays, and more.
- You can as well enquire the programme to provide yous with copies of your case file and the criteria, guidance, laws and any other information that formed the footing of their decision. Asking this information past calling your programme.
- Remember to keep copies of everything you submit and write down the names of anybody y'all speak to in the process.
If your need is urgent, you can ask for a "fast-tracked" entreatment.
Your plan has to make a decision within 30 days of receiving your appeal request. If yous asked for the appeal to be fast-tracked, your program must make a decision within 72 hours.
What if I lose my Plan Entreatment?
If you lose your Plan Appeal, you will receive a written deprival notice in the mail called a "Last Adverse Determination." This notice will explicate why the programme denied your care and give you a deadline and instructions for highly-seasoned the denial.
You have ii options to appeal the Final Adverse Determination, a Fair Hearing or an External Appeal.
- Y'all have 120 days from the engagement on the Final Adverse Conclusion notice to asking a Fair Hearing. At a Off-white Hearing, an Authoritative Law Judge will review your Medicaid managed care program'due south decision and your show to determine whether y'all and your provider accept proven that you run into the prior authorization standards for the service you need. A conclusion by the Administrative Law Judge is concluding and overrules whatever decisions past the plan. For more on how to request a Off-white Hearing and the Off-white hearing process, go to this Know Your Rights certificate here .
- An culling to a Off-white Hearing is an External Appeal. This entreatment is only bachelor if your service was denied for certain reasons, for example, if the plan said that your service was not medically necessary, experimental/investigational, or out-of-network. Your Concluding Adverse Determination volition state whether or not you have a right to an External Appeal. You take 4 months from the date on the Concluding Adverse Determination notice to asking an External Appeal. An External Appeal is completed entirely on newspaper. It will be reviewed by an independent external reviewer who is a trained physician. The reviewer will examine your evidence and the program'due south decision to decide whether the plan "acted reasonably and with sound medical judgment" and in your "best involvement." The external reviewer will upshot a decision within 30 days for a standard entreatment or 72 hours for an expedited appeal. If you lot have both a Fair Hearing and an External Appeal, the determination by the Administrative Police force Judge in the Off-white Hearing overrules any External Appeal conclusion. For more information or to file an External Appeal, go to the Department of Financial Services' website here .
How practice I appeal a Medicaid fee-for-service decision to deny my service?
If you have Medicaid fee-for-service and Medicaid has denied your service, your merely option to appeal the deprival is to asking a Fair Hearing. You have 60 days from the date on the denial observe to request a Fair Hearing. At a Off-white Hearing, an Administrative Law Estimate will review Medicaid's decision and your show to determine whether you and your provider have proven that yous meet the prior say-so standards for the service you demand. A decision by the Administrative Law Judge is concluding and overrules any decisions past Medicaid. For more on how to request a Off-white Hearing and the Off-white hearing process, become to this Know Your Rights document here .
Disclaimer
The information in this certificate has been prepared by The Legal Aid Gild for informational purposes just and is not legal advice. This information is not intended to create, and receipt of it does not establish, an attorney-customer human relationship. You should non act upon any data without retaining professional legal counsel.
Source: https://legalaidnyc.org/get-help/health-disability-hiv-aids/what-you-need-to-know-about-using-medicaid-to-get-health-care/
0 Response to "In Nj Will Medicaid Pay for a Family Member to Take Care of You?"
Post a Comment